Damaris Mutai
Medical Parasitologist
Medical Content Writer
Powered by Type
Cutaneous Leishmaniasis At A Glance
Cutaneous leishmaniasis is an infection of the skin that is caused by more than 20 species of Leishmania protozoans. It is spread to humans and animals through a bite from an infected female sandfly.
It causes painless skin lesions at the site of the sand fly bite. The lesions are often uncomplicated or self-limiting; they heal spontaneously. However, in severe cases, disfiguring and debilitating mucocutaneous leishmaniasis may arise.
What is the global health burden of cutaneous leishmaniasis?
Cutaneous leishmaniasis is a common type of leishmaniasis that affects many people globally in low and middle-income countries. According to WHO, 600,000 to 1 million new cases are reported yearly. However, these numbers may not be exact as most cases are underreported.
Overall, leishmaniasis is the third vector-borne disease of great global concern. The other top 2 diseases are malaria and lymphatic filariasis.
Geographic Distribution
- Sub-Saharan Africa: Algeria, Tunisia, Kenya, Uganda, Tanzania, Somalia Ethiopia, Cameroon, Senegal, and Sudan.
- The Americas- Brazil, Colombia, Peru, Bolivia, Panama, Costa Rica, Guyana, Guatemala, and Paraguay.
- The Middle East and South East regions- Saudi Arabia, Iraq, Iran, Afghanistan, Yemen, Bangladesh, and Pakistan.
What do Old and New World cutaneous leishmaniasis mean?
Old World cutaneous leishmaniasis (OWCL)
OWCL refers to leishmaniasis that is prevalent in sub-Saharan Africa, the Middle East, the Mediterranean, and distinct regions of Asia like India.
Oriental Sore, Aleppo boil, Delhi boil, Baghdad boil, Jericho boil, or tropical sore are some of the common names for OWCL.
The etiological Leishmania parasites are:
- L. major
- L. aethiopica
- L. donovani
- L. infantum
New World cutaneous leishmaniasis (NWCL)
NWCL is common in the limited parts of Mexico, South, and Central America.
American cutaneous leishmaniasis, pian bois, bush yaws, forest yaws, chiclero ulcer, and uta are some of the local names for NWCL.
The principal etiologic agents are:
- L. amazonensis
- L. mexicana
- L. braziliensis
The main difference between OWCL and NWCL lies in the disease vectors: infected female Phlebotomus and Lutzomyia sandflies are disease transmitters of OWCL and NWCL respectively.
Disease transmission
People in endemic regions can get a cutaneous infection following a bite from an infected female sandfly. The two important life cycle stages of the Leishmania parasites are the promastigote and the amastigote. These developmental stages target the macrophages, cells of the host immune cells.
A promastigote is an infective stage the sand fly introduces into the human or animal host during a blood meal. Blood is essential for egg production in sandflies.
By contrast, the amastigote is the tissue developmental stage of Leishmania. This is what the laboratory technician looks out for when undertaking various diagnostic tests like microscopy and biopsies.
There are 2 forms of leishmaniasis transmission:
Anthroponotic mode
Infected individuals serve as the parasite reservoirs, and thus are essential in the maintenance of the disease transmission cycle of human-sand fly-human. Needle sharing by intravenous drug users may lead to disease spread. Examples of the Leishmania parasites with this cycle are L. tropica and L. donovani.
Zoonotic mode
The transmission cycle of animal- sand fly- human requires animal reservoirs like dogs, hyraxes, armadillos, possums, and rodents.
The majority of the Leishmania parasites have this pattern; L. infantum, L. major, L. aethiopica in OWCL and L. mexicana, L. guyanensis, L.braziliensis, and L.amazonensis in the NWCL.
Read also Parasitic Zoonoses: What Are They?
Clinical presentations
The signs and symptoms vary depending on Leishmania species, geographic regions, host immune response, disease severity, and the parasites virulence factors.
The incubation period between infection and the first lesion appearance ranges from 2 weeks to 6 months. This is dependent on the parasite species. For example, L. major has a shorter incubation period of less than 2 months.
The 5 major types of cutaneous leishmaniasis are:
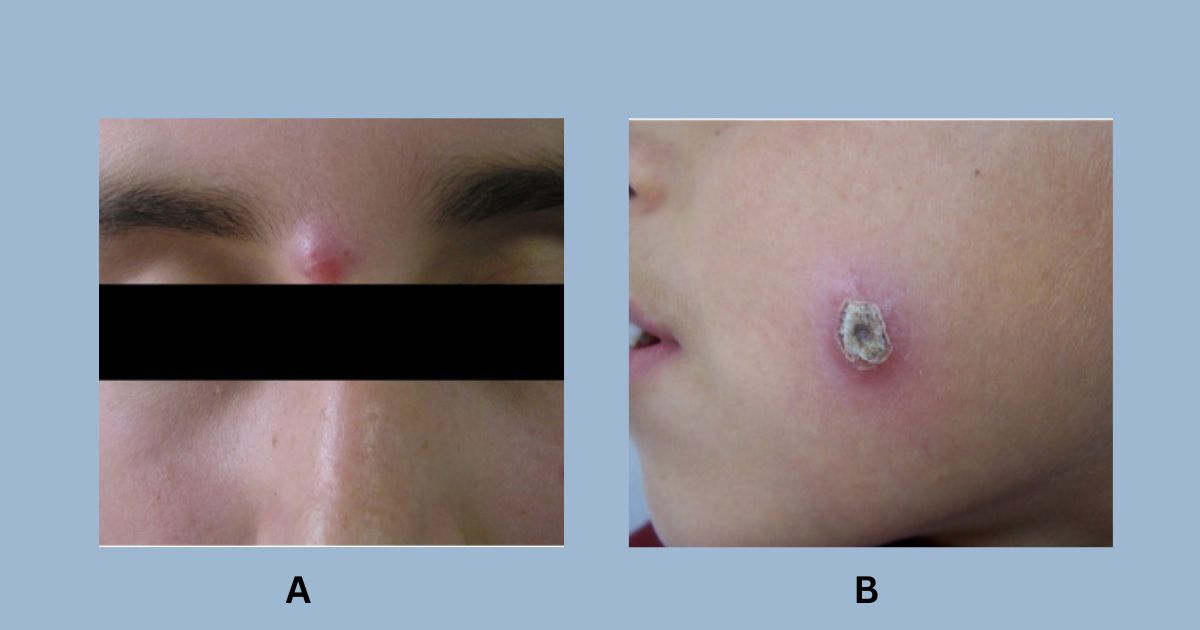
1. Localized cutaneous leishmaniasis (LCL)
Affected individuals often suffer from skin lesions at or near the sand fly bite area. The lesion may appear weeks, months, or even years after the initial infection.
The lesions can be found on the body parts that are mainly open and left exposed to the environment such as the face, lower legs, neck, or forearms. Recent research reports indicate that cutaneous leishmaniasis may also occur on the eyelids and male genitalia, particularly the glans penis.
Typical solitary localized lesions are common, however, multiple lesions that are large and locally destructive can also occur. These lesions are painless.
Initially, the skin lesions may appear after 2-8 months as a small red papule after which it slowly progresses to enlarge forming either an indolent ulcerated 2cm nodule or plaque within 6 months.
The formation of central ulceration called the volcanic ulcer with firm and raised borders is distinctive to cutaneous leishmaniasis. The identification of the distinct volcanic ulcer is essential for medical practitioners in ruling out other causes of chronic ulcers ad malignant tumors in leishmaniasis endemic regions.
Depending on the parasite species, the ulcers can be wet or dry. Wet LCL ulcers are larger, can exude pus, are prone to bacterial infections, and they do take a shorter time to heal spontaneously compared to dry LCL ulcers with crusted scabs.
Self-healing of the lesions may take 3-18 months. When healed, the lesions may leave hypopigmented atrophic scarring on the affected regions.
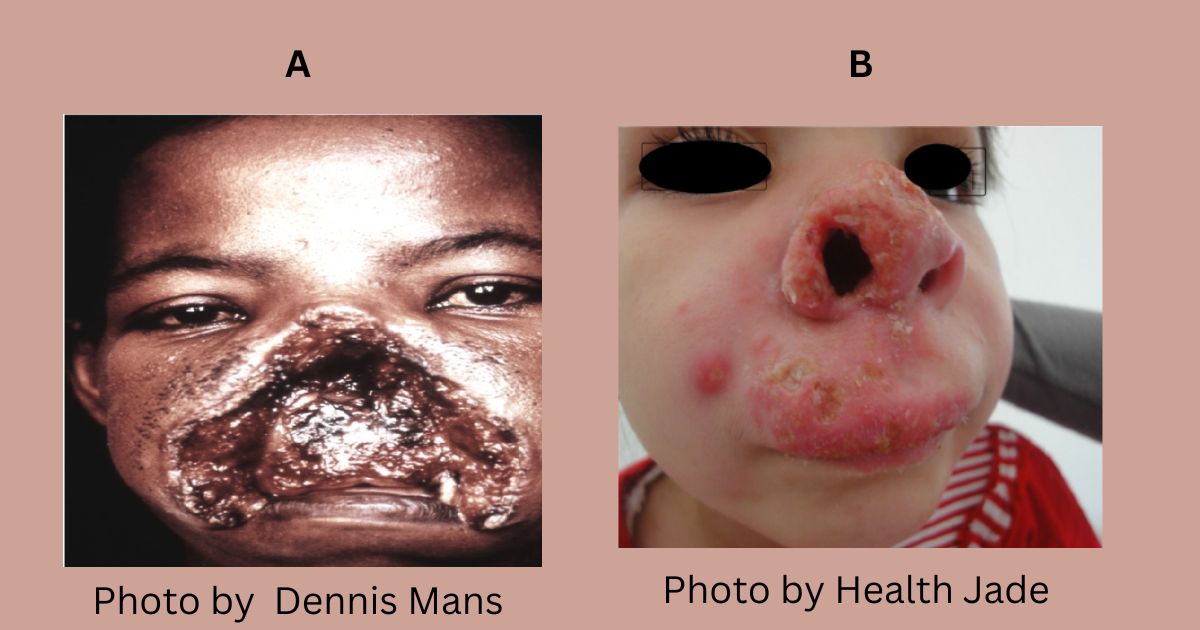
2. Mucocutaneous leishmaniasis or Espundia
Mucocutaneous leishmaniasis (MCL) is common in the New World. It arises following self-healing of LCL or healing of the initial LCL ulcers after successful local therapy.
The principal Leishmania parasites for MCL are:
- L.(Viannia). branziliensi
- L.(Viannia).panamensis
- L.(Viannia). guyanensis
MCL affects the mucous membranes of the nose, lips, palate mouth, or pharynx. The lesions are painful, inflammatory, and destructive in nature. Without treatment, extensive mucosal destruction due to tissue necrosis may arise resulting in permanent disfigurement, scarring, and life-threatening disabilities.
3. Anergic Diffuse cutaneous leishmaniasis (ADCL)
ADCL is a rare type of cutaneous leishmaniasis that majorly affects individuals with a weaker immune system. For example, HIV patients.
The causative agents for DCL are L.amazonensis and L. Mexicana in the New World and L.aethiopica in Kenya, Namibia, Tanzania, and Ethiopia.
DCL manifests as the occurrence of many nonulcerative nodular lesions on the body similar to those in lepromatous leprosy.
The initial nonulcerativate nodular lesion may occur on the extremities or the face. The spread of the lesions is slow and it may persist for many years in patients. As a result, more lesions further spread in the body.
The Leishmania parasites in the lesions grow uncontrollably and disseminate to other parts of the body via the lymhohematogenous route. Microscopic examination of lesion samples reveals a high concentration of amastigotes in the macrophages.
The hallmark of ADCL is T-cell anergy. This is an immune response state whereby the T helper immune cells are unable to elicit an immune response early enough against an antigen (in our case, the Leishmania parasite). This is the reason why ADCL patients have a negative Montenegro test or Leishmania skin test and are refractory to antileishmanial treatments.
4. Post- Kalazar dermal leishmaniasis (PKDL)
PKDL is a dermatological complication of the fatal form of leishmaniasis, visceral leishmaniasis due to L.donovani.
Its onset can be 6 months or within 10 years after recovery from visceral leishmaniasis. PKDL can also arise in patients who were not treated or were inadequately treated for visceral leishmaniasis.
The majority of PKDL cases happen in:
- India
- Bangladesh
- Nepal
- East Africa (Sudan, Kenya, Ethiopia)
PKDL manifestations are distinct to its geographic regions: It causes macular or hypomelanotic lesions in East African countries and papularnodular or polymorphic lesions in the South East Asia region.
It is important to note that lesions in African PKDL patients heal spontaneously. Patients only seek treatment for chronic lesions. On the contrary, Asian PKDL patients must seek treatment because their lesions are not self-healing.
The lesions are common on the face, the extremities joints, and the upper body, and rarely on the nose, tongue, and genitalia.

5. Leishmaniasis recidivans/ lupoid or relapsing leishmaniasis
Leishmaniasis recidivans is a rare variant of chronic LCL that recurs or forms new lesions within the edge of the primary lesion. Affected individuals may suffer from this clinical form of CL two or more years after the spontaneous resolution of LCL.
The lesions’ appearance varies from brown-red papules, psoriasiform lesions, and keloid plaques to verrucous lesions.
The amastigotes are absent in microscopy and cultures, therefore molecular tests like PCR are critical for clinical diagnosis.
Laboratory diagnosis
In suspected CL cases, the laboratory technician may request punch biopsy samples, and skin or mucosal lesion scrapings from the borders of active lesions.
There are several parasitological methods that are available for CL diagnosis.
- Microscopic examination for amastigotes in Giemsa or hematoxylin and eosin-stained thin lesion smears. Direct light microscopy is the gold standard diagnostic test.
- Leishmania intradermal skin test/ Montenegro skin test is useful in epidemiological surveys or vaccine trials. The test is a marker for the cellular immune response against Leishmania parasites. It identifies the level of T-helper immune response elicited via the measurement of delayed-type hypersensitivity skin reactions. The use of Montenegro test is on the decline due to the availability of alternative techniques.
- Molecular techniques have high specificity and sensitivity. Examples are PCR assays and loop-mediated isothermal reaction (LAMP).
- Serological methods- ELISA, lateral flow assays, Western blot, and direct agglutination tests.
- In vitro cultivation of promastigotes on Novy-MacNeal-Nicolle(NNN) medium or Scheider’s insect medium.
- Differential diagnosis is critical for distinguishing CL from other dermal infections with similar symptoms. The doctor may recommend other tests to rule out the diseases. For example, the skin lesions in hypopigmented macular PKDL are similar to those of lepromatomous leprosy, vitiligo vulgaris, and hypopigmented mycosis fungoides.
Treatment
Generally, there are fewer leishmaniasis therapies available.
- Pentavalent antimonials – sodium stibogluconate (Pentosam) and meglumine antimoniate( Glucantime) are the treatment of choice in endemic countries worldwide.
- Liposomal amphotericin B (AmBisome)
- Miltefosine (oral)
- Pentamidine
- Paromomycin
- Cryotherapy
- Heat therapy
Read also Current Trends on Leishmaniasis Treatments in Kenya
Take away
Cutaneous leishmaniasis is a neglected tropical disease that is not always in the limelight like infectious diseases including malaria and COVID-19. Despite the ‘unpopularity,’ the different clinical forms of the diseases should not be ignored. Public sensitization and education on prevention, treatment, and management are vital in curbing this emerging health problem.
Looking for Medical or Health-related Writing Services? Click Here
