Damaris Mutai
Medical Parasitologist
Medical Content Writer
Powered by Type
Everything You Need to Know about Toxoplasmosis
Toxoplasmosis is one of the neglected or ‘ forgotten’ parasitic infections that affect many people worldwide. It does not discriminate. In the US, for instance, it is the major cause of food-borne illnesses requiring hospitalization.
The infection affects people of all ages regardless of their age, sex, or immunity status. Expectant mothers, cat owners, and individuals with low immunity status are at the highest risk of suffering from the disease.
Although the mild form of the illness is self-resolving, chronic infections cause devastating health impacts like mental health-related problems, spontaneous abortions, respiratory failure, or even death.
Below are health facts on everything you need to know about toxoplasmosis.
What is toxoplasmosis?
Toxoplasmosis is a zoonotic parasitic infection caused by the obligate intracellular Toxoplasma gondii protozoans. This means that the infection is transmitted from animals to humans. The Felidae or the cat’s family, particularly the domestic cats, are the primary or definitive hosts for Toxoplasma gondii parasites. They can reproduce sexually only in the cat’s intestinal tract.

Toxoplasma gondii transmission facts
Humans can acquire toxoplasmosis through two main transmission modes: horizontal and congenital.
- Horizontal disease transmission occurs following accidental ingestion of Toxoplasma gondii oocysts or tissue cysts in contaminated foods, water, or the environment. Tissue cysts are usually present in the meat of sheep, goats, pork, raw oysters, mussels, or clams.
- Unwashed fruits or vegetables can also harbor oocysts.
- Raw goat’s milk from an infected goat suffering has also been documented to contain tachyzoites.
- Vertical or mother-to-child transmission results in congenital toxoplasmosis.
- Other routes include blood transfusion, organ transplants, bone marrow transplantation, sputum, semen, and breast milk
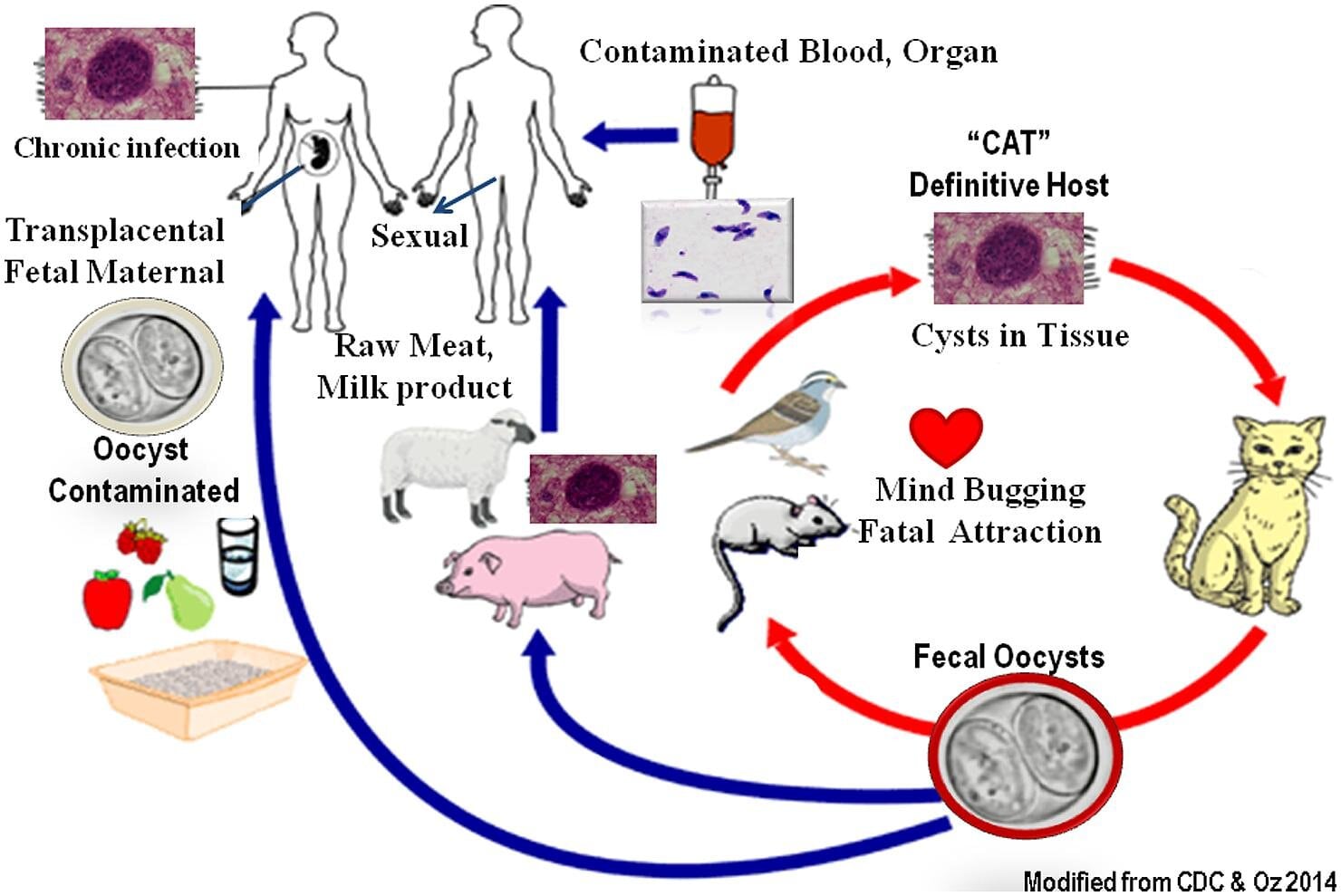
Disease transmission routes (Frontiers)
Toxoplasmosis statistics
Toxoplasmosis affects about 50% of the total world’s population. According to the World Health Organization, more than 1 million individuals from the European regions are infected with the disease each year. The major reason for the infection is food contamination with Toxoplasma gondii. More than 3,600 cases of vision loss and approximately 4,000 cases of congenital toxoplasmosis have been reported in the US.
What are the clinical presentations of toxoplasmosis?
Patients present different clinical signs and symptoms depending on their age, immunity status, gender, and disease severity.
Asymptomatic infection
The mild or acute form of the disease is asymptomatic. This means that many healthy individuals harboring the Toxoplasma gondii parasites do not exhibit any symptoms.
The hallmark clinical symptom of acute infection is lymphadenopathy. the disease causes the lymph nodes to swell due to the host’s immune response to fight against the Toxoplasma parasites.
The immunocompetent or individuals with a strong immune system may experience nonspecific flu-like symptoms that may last for several weeks, months, or even longer. These include:
- headaches,
- fever,
- sore throat,
- hepatosplenomegaly (swollen liver and spleen)
- muscle pains,
- self-resolving maculopapular rash
- ocular toxoplasmosis may result in impaired vision (these instances, however, are rare).
Symptomatic infection
Symptomatic chronic infection can arise due to the reactivation of the latent Toxoplasma gondii tissue cysts or disseminated toxoplasmosis. Reactivation often happens following the patient’s weakened immune system. Cancer chemotherapies, organ transplants, and AIDS (acquired immunodeficiency syndrome) are the key causes of low immunity status. The clinical form of the disease majorly affects the central nervous system and the eyes.
How does toxoplasmosis cause encephalitis?
AIDS patients are examples of target populations with a weakened immune system. AIDS is caused by the advancement of the Human Immunodeficiency Virus (HIV) infection to a chronic stage when left untreated. HIV attacks the CD4+ T-helper cells of the white blood cells in the patients resulting in a lower immune response to protect the body against the virus.
Toxoplasma gondii is an opportunistic infection in AIDS patients. The patients may suffer from life-threatening encephalitis. If the patients had previously acquired toxoplasmosis, Toxoplasma gondii present in the brain in its latent or inactive form is reactivated, causing extensive damage in the brain tissue and resulting in toxoplasmosis encephalitis.
Ho-Yen’s study’s findings demonstrated that 40% of the AIDS patient suffered from severe encephalitis. Approximately 10-30% of the immunosuppressed toxoplasmosis patients were reported to have succumbed to the illness. Nonetheless, the high percentage of toxoplasmosis encephalitis mortalities has been significantly reduced because of the introduction and widespread availability of highly active antiretroviral therapy (HAART) globally.
Patients with encephalitis may exhibit symptoms such as:
- poor coordination,
- difficulties of being alert
- muscle weakness
- confusion
- seizures
Effects of disseminated /extracerebral toxoplasmosis
The infection can spread to other organs in the body like the lungs. Individuals with disseminated pulmonary toxoplasmosis can suffer from pneumonitis. The overt clinical signs and symptoms include:
- breathing problems
- cough associated with fever, dyspnea, pulmonary rales, respiratory failure
- metabolic acidosis- a disease condition that is caused by the accumulation of acids in the body due to kidney failure or kidney infection.
- lack of treatment results in death
What are the clinical presentations of congenital toxoplasmosis?
Mothers can acquire the infection before or after conception. Congenital toxoplasmosis may result in spontaneous miscarriages, stillbirths, or congenital disabilities in newborns.
These congenital disabilities are:
- microcephaly (small head and brain)
- ocular retinochorditis- ocular lesions cause eye pain, blurred vision, teary eyes, and blindness if left untreated.
- jaundice (yellowing of the new-borns skin)
- calcification of the cerebrum,
- seizures,
- hydrocephalus (too much fluid accumulation in the brain),
- hearing problems,
- heart disorders
- retarded developmental growth milestones.
Although some congenital disabilities may not be evident immediately after the child’s birth, complications can arise later in their teenage or adult life, contributing to disability-adjusted years (DALY) conditions. DALY is the main cause of children’s overall lower quality of life.
How is toxoplasmosis diagnosed?
Routine clinical diagnosis of toxoplasmosis is made using serological tests. These are the laboratory diagnostic blood serum tests that measure the levels of antibodies produced to fight against the etiologic agents of a particular disease. Upon the Toxoplasma gondii immunoglobulin G (antigens) entry into human hosts, the body’s immune response involves activating the plasma immune cells to release IgA and IgM antibodies. These serological tests are:
- Western blot
- Latex agglutination tests (LAT))
- Sabin and Feldman dye tests (DT)
- Enzyme-linked immunosorbent assays (ELISA)
- Immunosorbent agglutination assays (ISAGA)- congenital toxoplasmosis
- chemiluminescence assays (CIA)
- indirect fluorescent antibody test (IFAT)
- piezoelectric immunoagglutination test (PAT)
Other diagnostic methods include:
Microscopy
Giemsa, hematoxylin, and eosin stains detect oocysts in cats’ feces, contaminated water, and environment settings such as soil.
Periodic acid Schiff stain identifies the amylopection granules of Toxoplasma gondii bradyzoites present fluid samples like goat’s milk.
Electron microscopy detects tissue cysts in the patient’s brain or the cat’s small intestinal tract.
Bioassays
Samples collected from patients, experimental animals, or meat tissues fed to cats play a critical role in diagnosing toxoplasmosis. Bioassay is the standard gold method for detecting Toxoplasma gondii pathogens in in-vitro experiments.
Molecular methods
These approaches are designed to detect the nucleic acids of Toxoplasma gondii parasites. Examples of the current useful molecular and genotyping methods are:
- Conventional polymerase chain reaction (PCR)
- Real-time PCR
- Loop-mediated isothermal amplification (LAMP)
- Microsatellite analysis
- High-resolution melting (HRM)
- Random amplified polymorphic DNA-PCR (RAPD-PCR)
- Multilocus sequence typing (MLST)
Imaging diagnostic approaches
The imaging techniques include computed tomography (CT) and magnetic resonance imaging (MRI). CT and MRI are useful in the detection of brain lesions and calcification. Ultrasonography is also crucial in the identification of hydrocephalus in infants.
Which medications are available?
Acute Toxoplasma gondii infections often do not require treatment. The immune system resolves the infection leading to the recovery of most infected individuals. However, medical attention in severe toxoplasmosis is warranted.
The first line treatment of toxoplasmosis is the pyrimethamine-sulfadiazine and folinic acid combination therapy for the active infection caused by the tachyzoites stage of the parasite. The drug kills Toxoplasma gondii protozoans by inhibiting dihydrofolate reductase and dihydropteroate synthetase enzymes responsible for the enzymatic action for folic acids synthesis of folic acids.
The following are alternative second-line toxoplasmosis chemotherapies:
- pyrimethamine-azithromycin
- , pyrimethamine-atovaquone,
- pyrimethamine-clindamycin
- pyrimethamine-clarithromycin
- atovaquone or trimethoprim-sulfamethoxazole monotherapies can also be used.
Spiramycin and pyrimethamine-sulfadiazine are the treatment of choice for prenatal acute maternal toxoplasmosis and established fetal toxoplasmosis, respectively.
Trimethoprim-sulfamethoxazole prophylaxis in HIV/AIDS patients co-infected with toxoplasmosis is useful in preventing the reactivation of the latent form of the disease.
All the above drugs are not effective against latent toxoplasmosis. There are no human vaccines that are currently available.
How can I prevent toxoplasmosis?
The following are the various control and prevention strategies:
- Avoid the consumption of undercooked or raw meat, including pork, mussels, lambs, oysters, and clams, for food-borne toxoplasmosis.
- Avoid the consumption of raw or unpasteurized goat’s milk.
- Maintaining high standards of food and overall personal hygiene to prevent the entry of Toxoplasma gondii parasites through the mouth. The hygiene practices include thorough hand washing and the use of clean drinking water both for drinking and cooking purposes.
- Promotion of health education programs in antenatal clinic visits and the community to sensitize the public on toxoplasmosis, particularly congenital toxoplasmosis.
- Screening of expectant mothers for toxoplasmosis in high-risk areas.
- Apart from tuberculosis, encephalitis, and hepatitis screening tests in immunodeficient patients, toxoplasmosis should be considered.
- Cat owners should ensure to clean their cat’s litter boxes daily. They ought to consider occasional veterinarian visits for toxoplasmosis screening.
- Wearing gloves during soil sampling or gardening.
Take away
Toxoplasmosis is one of the leading zones requiring patient hospitalization due to food-borne related illnesses. The devastating health impacts of toxoplasmosis, such as spontaneous abortions, encephalitis, microcephaly, and respiratory failure, illustrate the urgent need and attention for the development of feasible and fast treatment, control, and prevention for strategies for toxoplasmosis.
The non-specificity and subclinical signs and symptoms of acute toxoplasmosis make it difficult for individuals to be aware that they may be suffering from this parasitic infection. This means that seeking treatment for proper diagnosis and treatment in high-risk areas for toxoplasmosis is vital for managing the disease.
Further research on drug development and vaccines is vital to increase the number of treatment options for toxoplasmosis.

Great learning on Toxoplasma. This is an excellent command of knowledge!
Congratulations. On putting out there this piece of work.
I am personally interested in Toxoplasmosis and I am currently looking at how we can target stage conversion between disease causing tachyzoites and latent bradyzoites for chemotherapy
Kudos! Damaris
Thanks Edwin, we can collaborate in toxoplasmosis research someday. i’d love to hear more regarding toxoplasmosis research in real research setting
Wonderful teaching……keep the spirit
Thank you Austine