Damaris Mutai
Medical Parasitologist
Medical Content Writer
Powered by Type
Schistosoma haematobium: Understanding The Disease It Causes
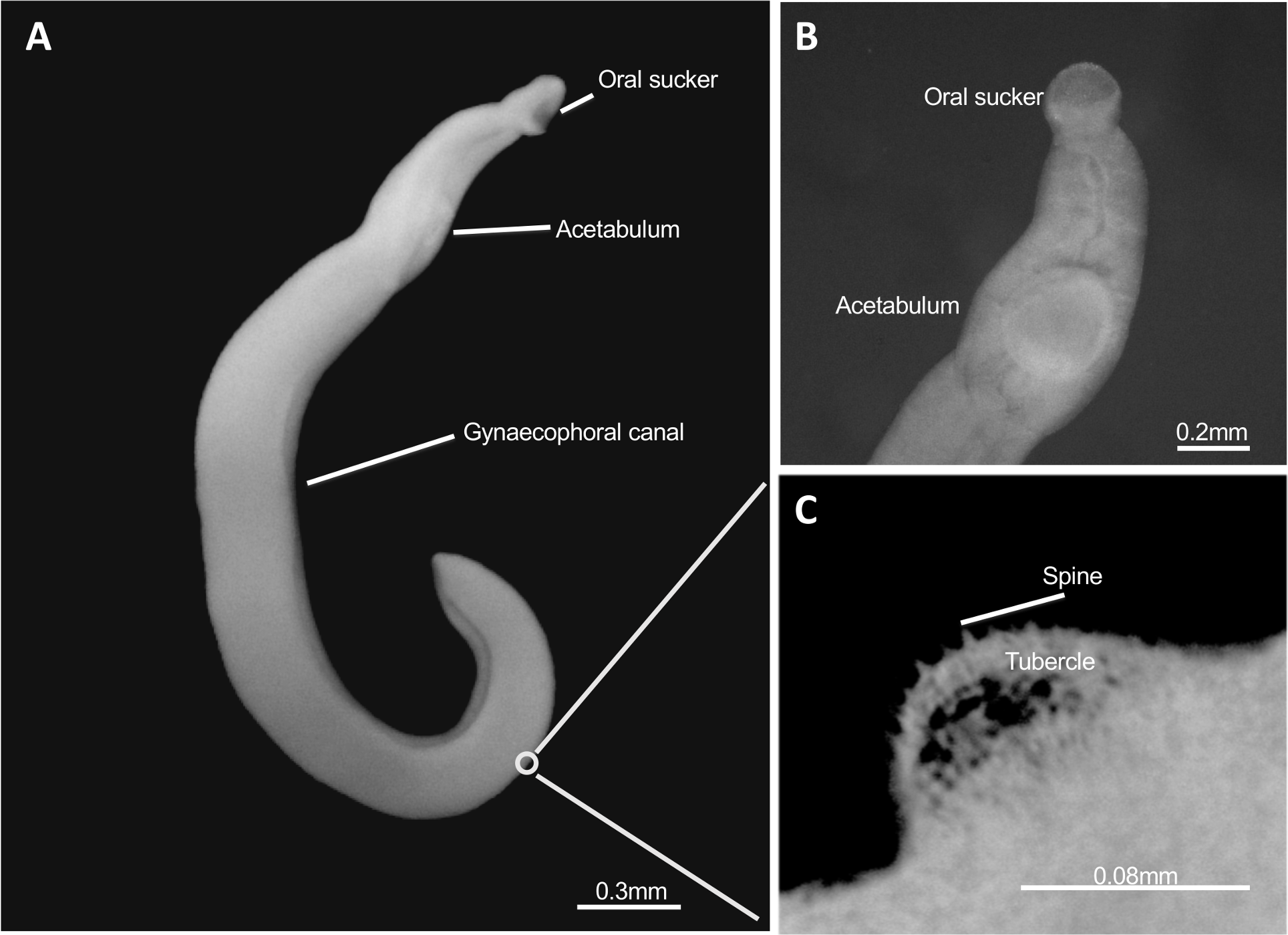
Schistosoma haematobium (S. haematobium) is one of the blood flukes or flatworms responsible for causing urogenital schistosomiasis. This is a parasitic disease that affects the urinary tract system and the reproductive organs of men and women.
The predilection sites of S. haematobium in the urinary tract system include the urinary bladder, ureters and the urethra. the
Apart from the aforementioned urinary tract target sites, the bladder fluke may also affect parts of the female reproductive system. Examples are the uterus, fallopian tube, ovaries, vulva, vagina, and the perianal region.
However, in men, it is known to negatively affect the functionalities of the prostate, seminal vesicles, and scrotum.
There are two major forms of S. haematobium infections namely:
- Female genital schistosomiasis (FGS)
- Male genital schistosomiasis (FGS)
Who are at the greatest risk?
Individuals who have high chances of suffering from urogenital infections are those who frequently come in contact with freshwater bodies infested with Bulinus freshwater snails harboring the parasite. Bulinus species are the intermediate hosts of S. haematobium vital in its life cycle.
Infection can occur while undertaking daily water-related domestic chores, bathing, swimming, or economic activities like fishing
These groups of individuals are:
- Women of childbearing reproductive age
- Children aged between 3-13 years
- Fishermen
Geographic Distribution
Schistosoma haematobium is endemic to Sub-Saharan Africa, the Middle East, and Corsica in France. It is prevalent in low and middle-income countries with freshwater bodies like lakes and rivers.
The high prevalence of the infection in these regions is strongly linked to high levels f poverty, poor sanitation, and inadequate access to potable water.
How does S. haematobium cause infection?
Before we delve further into the pathogenesis of urogenital schistosomiasis, let’s have a preview of the parasite life cycle.
Poor sanitation such as lack of access to toilet use may force an individual to urinate in lakes or rivers. If the individual was suffering from urogenital schistosomiasis, he/she is more likely to shed S. haematobium eggs in urine.
These eggs then hatch releasing ciliated miracidium into the lake. Miracidium remain infectious to the specific intermediate freshwater snail for 6-12 hours. Consequently, the miracidium swims through ciliary action scouting for the Bulinus freshwater snail and penetrate its tissue ,thus infecting the snail. It looses its cilia upon penetrating the snail tissue.
In the snail, the miracidium changes to a mother sporocyst that subsequently undergoes two propagative asexual reproduction stages resulting in the formation of daughter sporocysts. The daughter sporocysts then migrate to the hepatic and gonadal tissues of the snail. they do also continue to develop in these tissues and within 2-4 weeks they result in of a forked-tailed S. haematobium stage called cercariae. The Bulinus freshwater snail finally releases the cercariae into the water whereby it awaits its next host.
Following a person skin contact’s with a contaminated freshwater lake infested with infected Bulinus snails, the cercariae penetrate the skin into the human body. Cercariae loses its tail in the process and becomes schistosomulae. it takes 2 and 3 days for the schistosomulae to reach the skin dermis and the dermal blood vessels respectively.
Schistosomulae migrates in the human through venous circulation. During circulation, it moves through the lungs ,heart, and finally into the liver where it matures to into adult bladder worms. Upon maturation, it migrates via the portal vein into the venous plexus of the urinary bladder. In the 9th week they copulate and the female lays eggs which are subsequently excreted in urine and the cycle continues. The females can lay up to 300 eggs per day but only 150 of these eggs are shed off .
The passage of schistosomal eggs of the parasite into the genitourinary tissues elicit an inflammatory immune response that cause damage to the tissues and organs.
Clinical signs and symptoms
The signs and symptoms of urogenital schistosomiasis vary with the disease severity: they can range from mild dermatitis to chronic infections.
Within 1 hour of skin contact with cercariae, an individual may experience mild dermatitis and a rash at the schistosomulae entry site into the body.
The typical clinical manifestations are dysuria (painful urination) and hematuria (presence of blood in urine).
Just like toxoplasmosis, female genital schistosomiasis cause dire health consequences in women and expectant mothers. Male Genital Schistosomiasis and Female Genital Schistosomiasis cause distinct clinical signs and symptoms.
In early stages , afflicted men may experience:
- Pelvic, coital ,or ejaculatory pain,
- Abnormal ejaculation,
- Haemospermia ( presence of blood in semen).
- Abnormal swelling of the male reproductive organs including seminal vesicle and prostate gland.
As the S. haematobium infection progresses to chronic stages, it increases the risk of men suffering from:
- Primary or secondary infertility
- Chronic kidney disease
- Kidney failure
- Iron deficiency anemia
- Urinary bladder cancer
On the other hand, women suffering from acute female genital schistosomiasis may experience :
- Vaginal itching and bleeding
- Swelling and ulcerations of the vulva and vagina
- Genital lesions- may appear as grainy sandy patches, homogenous yellow patches or rubbery papules
- Bloody or abnormal smelly vaginal discharge
- Dyspareunia( persistent coitus experience
- Stress incontinence ( urine leaks)
In the long-term, FGS may increase the risk of:
- Ectopic pregnancy, spontaneous abortion, premature birth or low birth weight babies
- Primary or secondary infertility
- Human Immunodeficiency Virus(HIV)
- Human papillomavirus infection(HPV
- Chronic kidney disease
- Cervical cancer
- Iron deficiency anemia
- Social stigma and discrimination
Watch the video below on real life experiences of Kenyan women and girls with FGS as highlighted by the local news broadcast, the Citizen TV Special Report.
Which diagnostic tests are in place?
Diagnosis of urogenital schistosomiasis is typically made through a combination of physical examination, urine tests, and imaging studies.
The gold standard test for urogenital schistosomiasis infections is urine microscopy for S. haematobium eggs or ova. Microscopy is useful, particularly in resource-limited settings. It is cheap and easy to perform. Through microscopic urine examination, the laboratory technician can determine the disease severity using egg counts.
Other diagnostic tests are:
- Reagent urinalysis dipstick
- Serological assays- high eosinophil levels indicate acute infection while elevated renal or liver functions suggest a chronic infection
- Biopsy of genital tissues
- Molecular methods such as real-time PCR
What are treatment options for S. haematobium infections?
Praziquantel is the current antiparasitic treatment choice for urogenital schistosomiasis.
Praziquantel is effective only against adult S. haematobium worms but not juvenile ones. The lack of efficacy against young schistosomal worms is the key reason for low cure rates in hyperendemic regions.
What are control and prevention strategies?
- Avoiding contact with contaminated water sources.
- Promoting and diversifying the adoption of WASH( Safe drinking- water, sanitation, and hygiene) projects both at the local and national levels in endemic areas
- Wearing protective clothing while undertaking economic activities such as fishing
- Washing hands thoroughly after coming into contact with contaminated water.
- Increasing awareness both to the public and health care professionals on urogenital schistosomiasis-WHO 2015 Female Genital Schistosomiasis Pocket Atlas is already available
- Training of healthcare professionals on Female and Male Genital Urogenital schistosomiasis
- Prompt diagnosis and treatment of suspected haematobium infection with praziquantel
- Integration of urogenital schistosomiasis screening in reproductive health clinical services in endemic regions. Urogenital schistosomiasis will be an addition to clinical screening services like family planning, STI/HIV, and cervical cancer.
Way Forward
S. haematobium causes urogenital schistosomiasis, a serious and potentially debilitating parasitic infection that can have a significant impact on the health and well-being of those affected. It is important to be aware of the symptoms of the disease and to take steps to prevent its spread. With prompt and effective treatment, most people with urogenital schistosomiasis can recover fully and go on to lead healthy, active lives.

A great article…
Thank you for the feedback